Behavioral health: Strategic priorities
Sending proven interventions into action: Expanding access to mental health and substance use disorder treatment
Following several years of trying to restore funding that was cut deeply during the Great Recession, Gov. Inslee launched a plan in 2018 to transform Washington’s behavioral health system. The rebuilding and transforming is paying off. New facilities and various reforms have reduced wait times for certain behavioral health services from months to days. An innovative new teaching hospital at the University of Washington opened this year, and the state broke ground on a new forensic hospital in Lakewood. Thousands of people are able to find care in their own communities at new facilities.
Washington’s growing population — combined with the urgent risks posed by opioids, such as fentanyl — require continued action. Any reductions will slow this progress. That’s why Gov. Inslee’s 2025–27 biennial budget continues delivering proven solutions and community-based care. This is especially important for communities disproportionately impacted by stigma and other barriers to accessing appropriate services.
Need:
Proposal:
Continue filling gaps in behavioral health capacity
Treatment for mental illness and substance use disorder requires a wide range of specialized services and care. When there are gaps in the system, people fall through them. That’s why the state has been building and opening facilities that provide specialized care when and where people need it.
To meet needs and save lives, Governor Inslee’s budget continues investments in state capacity to treat patients and in community-based care. This includes services at state-funded hospitals and behavioral health facilities, with new construction such as the Brockmann campus in Clark County and the Forensic Center of Excellence at Western State Hospital. The newly opened UW Behavioral Health Hospital provides care and treatment, while also serving as a teaching hospital to train future behavioral health practitioners.
With opioid-related deaths continuing to rise rapidly in Washington state, funds are urgently needed to apply proven strategies for connecting people to treatment and recovery. The 2025–27 operating budget adds $22 million, all obtained through opioid-related settlements, to fund these services funding for these services. Examples include providing medications for opioid use disorder in emergency departments and schools. The state is also pursuing strategies to expand treatment and support more youth and young adults, pregnant people, and communities disproportionately impacted by the opioid crisis. Fern Lodge Behavioral Wellness in Stanwood, for example, will provide culturally sensitive healing and support through a partnership with the Tulalip Tribes. In the capital budget, a new $20 million investment from the State Building Construction Account is added for a substance use disorder clinic in Poulsbo that will help serve the Suquamish Tribe and neighboring communities in Kitsap County.
An ecosystem of behavioral health care that spans prevention and early intervention all the way through treatment and recovery leads to a healthier, safer Washington. We’re building on what works — making it easier to get the care that people need, at the right time and in the right place.
Community-based long-term civil commitment (LTCC) capacity
To better meet people’s needs, Washington state is building an ecosystem of community-based care while also increasing capacity at state-run facilities. This approach will help people connect with services earlier, closer to home, and at the appropriate level of care for their needs.
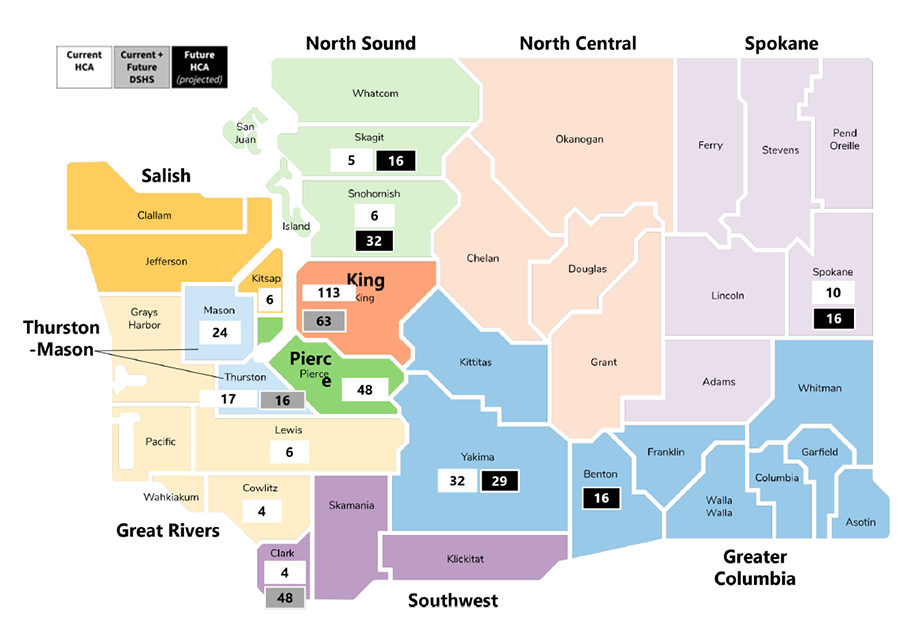
The map below shows the locations and estimated numbers of community-based long-term civil commitment (LTCC) beds by county, based on data available in November 2024. It includes:
- 275 beds currently contracted by the Health Care Authority (HCA) for fiscal year 2024
- 79 beds currently owned and operated by the Department of Social and Health Services (DSHS)
- 48 future beds planned at facilities owned and operated by DSHS
- 109 future beds projected for HCA contracts
The projected future total comes to 511 beds based on current plans. Counties still in need include Spokane, Benton, Chelan, Whatcom, Kitsap, Grays Harbor, and Clark.
Behavioral health budget highlight items
Support Tribal opioid prevention and response
Tribes and Urban Indian Health Programs are on the frontlines of opioid and overdose response. American Indian and Alaska Native people are five times more likely to die from synthetic opioids, like fentanyl, than the general population in Washington state. Funding is urgently needed to save lives. Governor Inslee’s budget includes funding to support Tribal efforts to reduce opioid misuse, overdoses, and deaths. Tribes may use the funds for culturally relevant prevention, outreach, treatment, recovery support services, and other strategies to address and mitigate the effects of the misuse and abuse of opioid-related products.
($16.4 million Tribal Opioid Prevention and Treatment Account)
Expand access to medication for opioid use disorder in emergency departments
Washington state emergency departments had more than 24,000 visits for nonfatal overdoses in 2022. For people with opioid use disorder, these encounters are critical opportunities for intervention. Of patients who visit the emergency department for nonfatal overdose, 5%–8% die in the year following discharge, and 20%–30% of patients who die do so in the first month. Medication for opioid use disorder (MOUD) treatment in the emergency department reduces mortality rates by up to 63%, yet less than 9% of emergency department opioid overdose patients receive a prescription for buprenorphine. Emergency department bridge programs, which connect patients to follow-up care in and beyond the emergency department, are effective interventions that increase rates of MOUD initiation and decrease rates of mortality. Gov. Inslee’s budget funds a statewide program that will make it easier
for emergency department clinicians to prescribe MOUD. It provides all Washington state EDs with real-time MOUD clinical guidance and 24/7 follow-up appointment scheduling. Enrollment is voluntary, free, and open to all Washington hospitals and pre-hospital systems.
($758,000 Opioid Abatement Settlement Account)
Decrease housing instability for young adults exiting state care
Many young adults between the ages of 18–25 are at high risk of homelessness when they leave inpatient behavioral health facilities. To support these young people through this critical transition, the 2024 supplemental budget funded two short-term housing programs, one on each side of the mountains. The governor’s 2025–27 budget adds two more facilities, one in Northern Washington, and one in Southern Washington, to expand these services and help more of these young adults.
($6 million GF-S)
Support personal care for people with behavioral health conditions in community living facilities
Community Behavioral Health Supports (CBHS) is replacing Behavioral Health Personal Care (BHPC). This program helps individuals who have a significant mental health diagnosis and need additional support to live in a community setting, such as an adult family home, assisted living facility, or enhanced services facility. Services are provided by staff who assist clients with structure, safety, social engagement, and community activities. In many cases, this support helps individuals transition from an inpatient psychiatric setting to a community setting.
($54 million GF-S, $52 million GF-F)
Increase access to care by Certified Community Behavioral Health Clinics
Certified Community Behavioral Health Clinics (CCBHCs) are designed to ensure access to coordinated, comprehensive behavioral health care. CCBHCs are required to get people into care quickly and serve anyone who requests care for mental health or substance use — regardless of ability to pay, place of residence, or age. This includes developmentally appropriate care for children and youth.
CCBHCs must meet federal standards for services and are required to provide:
- Crisis services available 24 hours a day, seven days a week.
- Comprehensive services, so patients don't have to piece together the behavioral health support they need across multiple providers.
- Care coordination to help people navigate behavioral health care, physical health care, social services, and other relevant systems of care.
Funding will continue CCBHC expansion and develop a rate structure for providers in Washington state.
($1.2 million GF-S)
Expand services for Trueblood class members
The governor’s budget provides funding to implement the Phase 4 settlement under Trueblood, et al. v. Department of Social and Health Services, et al. Funding is provided to increase outpatient competency evaluations and restoration, crisis stabilization and housing, and connections to behavioral health services.
($59 million GF-S)
Serve more people at University of Washington Behavioral Health Hospital
Since opening in July 2024, the new University of Washington Behavioral Health Hospital has been providing behavioral health services to individuals receiving inpatient psychiatric care for 90- and 180-day civil commitments. Funding is provided as the UW Behavioral Health Hospital builds up to utilizing all 75 long-term civil commitment beds so that more people can receive the care and treatment they need.
($18.5 million GF-F)
Provide opioid use disorder education and treatment in juvenile rehabilitation settings
Young people entering juvenile rehabilitation facilities come with increasingly complex behavioral health challenges, including opioid use disorder (OUD). The demand for MOUD treatment and overdose prevention has outpaced DCYF’s current resources. Additional funds will enable medical personnel to provide MOUD education and treatment.
($1.3 million Opioid Abatement Settlement Account)
Leverage telehealth to connect people with opioid use disorder treatment
Gov. Inslee’s budget funds a statewide program that will help more Washingtonians connect with the treatment they need. Through a partnership between the Department of Health (DOH) and University of Washington Department of Emergency Medicine, this program will provide free, on-demand telehealth visits 24 hours a day, seven days a week. Visits include support from Linkage to Care Coordinators, who will assist patients with connections to care within 72 hours of their first visit.
($3.2 million Opioid Abatement Settlement Account)
Raise awareness about opioid risks for people who are currently or were recently pregnant
Washington state is home to 54 birthing hospitals and many doulas, lactation counselors, and community health workers who provide services to individuals during and after pregnancy. This budget provides funding for a communications campaign that raises awareness about perinatal behavioral health and opioid risks. It will provide high quality training materials to all 54 birthing hospitals, enhance Tribal lactation guidelines, and provide training for doulas and community health workers.
($410,000 Opioid Abatement Settlement Account)
Improve capacity and safety at state hospitals
The governor’s proposed budget funds construction, preservation, and maintenance of state hospitals. For Western State Hospital, funding includes the final phase of construction for the new 350-bed Center of Excellence. Gov. Inslee’s proposal also funds projects necessary for health and safety at existing buildings at Western State Hospital and Eastern State Hospital. The investment addresses needs such as fire alarm replacements, water system assessments, and transformer repair.
($333 million State Building Construction Account)
Improve safety and usability at state-funded behavioral health facilities
In addition to state hospitals, Washington’s behavioral health facilities provide care to people outside of hospitals. This capital budget invests in modernization and renovation to ensure that these facilities remain safe and available for those who need them. Funding will support projects such as construction of security enclosures and renovation of recreational yards.
($45 million State Building Construction Account)
Expand capacity for community-based behavioral health care
To get well, people need easy access to appropriate levels of care at the right time and in the right place. For most, the best place is in or near their community. Gov. Inslee’s budget continues to expand access to behavioral health services by investing in community-based care. Funds will be used to award grants to community hospitals and providers for the establishment and expansion of services such as crisis relief centers, peer respite care, long-term facilities for youth and older adults, secure withdrawal management, and stabilization treatment. For example, funding will help to set up a substance use disorder clinic in Poulsbo to support regional needs.
($107 million State Building Construction Account)
Behavioral health summary of investments, 2025-27 biennial
This document highlights select investments proposed by the governor for opioid use disorder response and behavioral health. The chart below provides the full list of investments. For more details about the items in the chart, refer to the Budget Recommendation Summaries (Rec Sums), organized by agency.
| Focus Area | Items | Agency | Amount |
|---|---|---|---|
| Opioid use disorder | Tribal Opioid Prevention and Response | HCA | $16,381,000 |
| Emergency Department MOUD | HCA | $758,000 | |
| Juvenile Rehabilitation MOUD | DCYF | $1,302,000 | |
| Telehealth Link to MOUD | DOH | $3,150,000 | |
| Perinatal Opioid Use Disorder Education and Awareness | DOH | $410,000 | |
| Total | $22,001,000 | ||
| Behavioral health | Young Adult Discharge Program | HCA | $6,000,000 |
| Community Behavioral Health Supports | HCA | $106,395,000 | |
| Certified Community Behavioral Health Clinics | HCA | $1,236,000 | |
| Trueblood Phase 4 Settlement Agreement | HCA | $59,083,000 | |
| UW Behavioral Health Hospital | HCA | $18,538,000 | |
| State v. Blake Projects and Programs | HCA | $19,129,000 | |
| Behavioral Health Personal Care Waiver | HCA | $32,000 | |
| SB5236 Staffing Requirements | DSHS-BHA | $1,031,000 | |
| Trueblood Legislation | DSHS-BHA | $1,028,000 | |
| Total | $212,472,000 | ||
| Capital | State Hospitals | DSHS | $333,000,000 |
| Behavioral Health Facilities | DSHS | $45,000,000 | |
| Behavioral Health Community Capacity | Commerce | $107,000,000 | |
| Total | $485,000,000 | ||
| Grand Total | $719,473,000 |


